Consent questions will be added at 72 hours and discharge (Section 3 and 7).
Consent question in Section 3: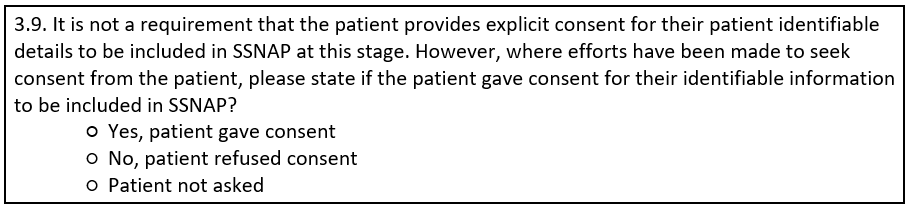
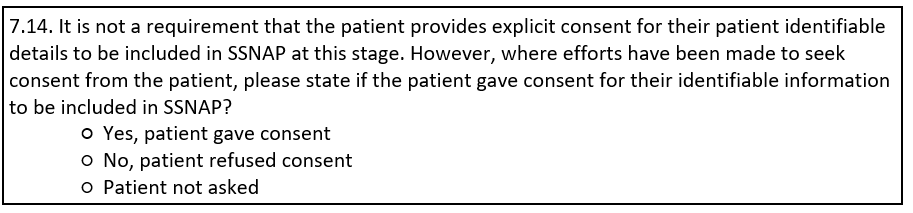
Consent question in Section 7:
FAQs:
Do teams in Northern Ireland still need to answer these questions?
Teams in Northern Ireland do not have to ask for consent as no patient-identifiable data is submitted to SSNAP. These teams can say "patient not asked" by default to the new consent questions (as listed above).
What happens to patients who are too unwell to give consent within the 72 hours?
SSNAP currently has approval under Section 251 to collect confidential information up to six months after a patient has had a stroke, and so it is not a requirement that the patient is asked for consent at this stage. If the patient was not asked for consent or they could not give consent, please record “patient not asked”.
Does asking/not asking for consent affect scoring?
It is not a requirement that the patient is asked for consent in the first 72h or by discharge. Teams will not be scored on whether or not they ask for consent.
If a patient has consented in the acute setting for patient identifiable information to be recorded on SSNAP (in section 3) do teams need to check again when the patient is being discharged (Q in section 7)?
The consent question in Section 7 will only be available if 'Patient not asked’ is selected for the question in section 3. It will be set up on the webtool so that if the patient has consented at any point in the pathway then this will be flagged to later teams, who will not have to ask the question again.
If the patient doesn't consent to share patient identifiable information, how is the record transferred to community providers?
You can still transfer the record on SSNAP and contact the community team to let them know that this patient does not have identifiable information. The patient will still have a unique SSNAP ID that can be used to search the patient on the SSNAP webtool.
How do you anonymise the patient identifiable data on SSNAP?
Once “No, patient refused consent” is chosen for a consent question, the webtool will remove all patient identifiable information. The team does not need to do anything else. This includes: name, NHS number, hospital number, date of birth and postcode. The patient will still have a unique SSNAP ID that can be used to search the patient on the SSNAP webtool.
If a patient does not consent, can we still start a record?
If you ask a patient for consent for their identifiable data to be added to SSNAP before you have started their SSNAP record but the patient does not consent, their record should not be started on SSNAP. To start a record teams have to enter patient-identifiable data onto the SSNAP record (name, NHS number, post code). If a patient has not consented to this the record should not be started.
If after you have added the record onto SSNAP you ask for the patient's consent and the patient refuses, please answer 'No, patient refused consent'. Once you answer 'No, patient refused consent' all patient-identifiable data will be automatically wiped from the webtool.
Are there patient information leaflets available to download and give to patients when discussing consent?
Patient information sheets are available here: https://www.strokeaudit.org/Patients,-Carers-Public-Area/What-data-does-SSNAP-collect.aspx